 Clomiphene Vs. Other Fertility Drugs: Pros and Cons
Clomiphene Vs. Other Fertility Drugs: Pros and Cons
Clomiphene: Cost-effective Yet Potent Fertility Treatment Option
Affordability
Effectiveness
Clomiphene is an inexpensive option, making it accessible to many couples seeking fertility treatment. Its cost-effectiveness is a major advantage, allowing multiple treatment cycles without breaking the bank.
Despite its affordability, clomiphene boasts impressive efficacy in inducing ovulation and improving pregnancy rates. Its potent mechanism of action makes it a reliable first-line therapy for couples struggling with infertility.
Clomiphene has emerged as a game-changer in the world of fertility treatments, offering a unique combination of cost-effectiveness and potency. Its affordability allows couples to explore multiple treatment cycles without financial strain, while its clinically proven efficacy ensures a promising path to parenthood. As a first-line therapy, clomiphene has become a trusted ally for many couples embarking on their fertility journey.
Side Effects: Balancing Efficacy with Potential Risks

While clomiphene offers an effective and affordable fertility treatment option, it's crucial to weigh the potential side effects. Mild side effects like hot flashes, headaches, and mood changes are common, but more severe risks like ovarian hyperstimulation syndrome or multiple pregnancies cannot be overlooked. Careful monitoring and open communication with healthcare providers are essential to balance the potential benefits and risks.
Clomiphene primarily works by stimulating the release of hormones that trigger ovulation. However, this disruption in the delicate hormonal balance can lead to undesirable side effects. Fortunately, many women tolerate clomiphene well, but those with pre-existing conditions or a history of ovarian cysts may require closer monitoring.
Ultimately, the decision to proceed with clomiphene should be made in consultation with fertility specialists, weighing individual circumstances, medical history, and personal preferences. A personalized approach ensures that the benefits outweigh the potential risks, maximizing the chances of a successful and healthy pregnancy.
Ovulation Induction: Unveiling Clomiphene's Mechanism of Action
Clomiphene, a synthetic estrogen modulator, works by stimulating the release of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) from the pituitary gland. This hormonal surge triggers the growth and maturation of ovarian follicles, leading to ovulation. As a relatively inexpensive and well-tolerated medication, clomiphene has become a popular first-line treatment for ovulatory dysfunction.
By mimicking the body's natural hormonal signals, clomiphene helps restore the delicate balance required for successful ovulation. This mechanism of action makes it an attractive option for women struggling with anovulatory infertility or irregular ovulation patterns. However, it's important to note that clomiphene's efficacy may diminish with prolonged use due to potential receptor desensitization.
Careful monitoring and timely adjustments by a fertility specialist are crucial for optimizing treatment outcomes with clomiphene. Tracking follicular development through ultrasound and appropriate timing of intercourse or fertility procedures can significantly increase the chances of conception.
Exploring Alternative Fertility Drugs: Gonadotropins and More

While clomiphene remains a cost-effective and widely used option, other fertility drugs, such as gonadotropins, offer alternative approaches. Gonadotropins, like follicle-stimulating hormone (FSH) and human menopausal gonadotropin (hMG), directly stimulate ovarian follicle growth and ovulation. These medications are often used in cases where clomiphene is ineffective or for more advanced assisted reproductive techniques like in vitro fertilization (IVF).
Additionally, aromatase inhibitors like letrozole have emerged as potential alternatives to clomiphene, as they may have fewer side effects and better success rates in certain patient populations. Exploring these options with a fertility specialist can help determine the most suitable treatment plan based on individual circumstances and preferences.
Personalized Approach: Choosing the Right Fertility Treatment
When it comes to fertility treatments, a personalized approach is crucial. Factors such as age, medical history, and underlying causes of infertility must be carefully considered. While clomiphene remains a cost-effective and widely used option, other fertility drugs, like gonadotropins or injectable medications, may be more suitable for certain individuals.
Fertility specialists meticulously evaluate each case, weighing the benefits and risks of various treatment options. This comprehensive assessment ensures that the chosen therapy aligns with the patient's specific needs, maximizing the chances of success while minimizing potential side effects.
Ultimately, open communication between patients and healthcare providers is key. By fostering a collaborative environment, couples can make informed decisions and embark on a fertility journey tailored to their unique circumstances.
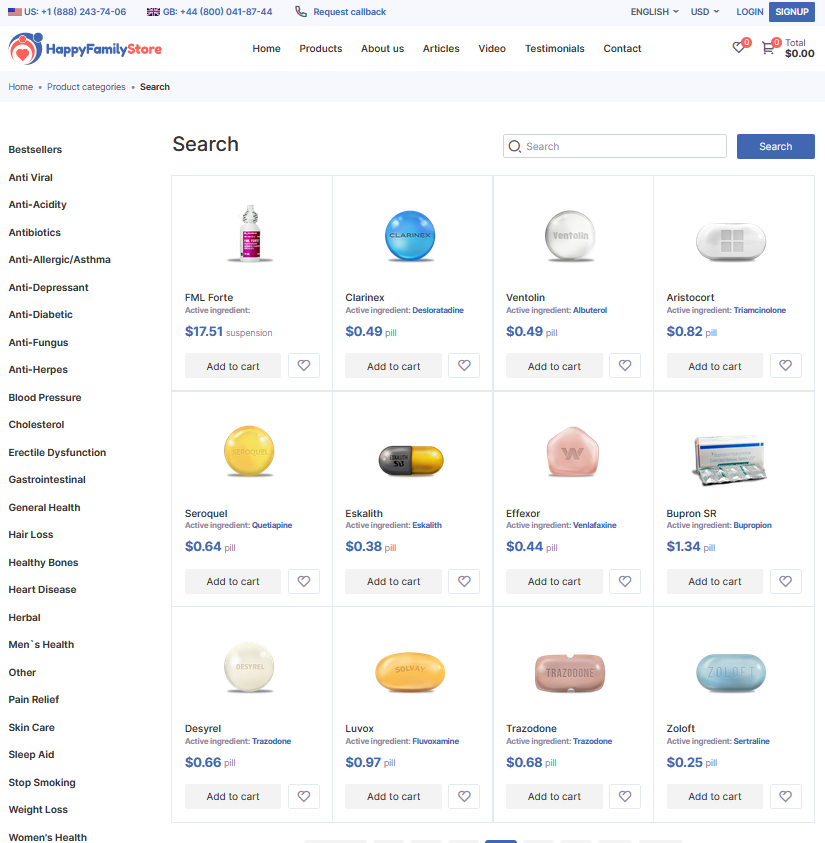
| Drug | Cost | Success Rate |
|---|---|---|
| Clomiphene | Low | 20-40% |
| Gonadotropins | Moderate | 30-50% |
| IVF | High | 40-60% |
Success Rates: Real-world Data on Pregnancy Outcomes
When it comes to evaluating fertility treatments, success rates based on real-world data provide invaluable insights. Studies have shown that clomiphene citrate, a widely used ovulation-inducing medication, has a respectable success rate, particularly for women with unexplained infertility or polycystic ovary syndrome (PCOS). However, success rates can vary significantly depending on factors such as age, underlying causes of infertility, and treatment protocols.
It's important to note that success rates are often reported as "live birth rates" rather than just pregnancy rates, as the ultimate goal is a healthy, full-term pregnancy. Research indicates that with clomiphene treatment, live birth rates range from 10% to 20% per cycle, with slightly higher rates in younger women and those with less severe infertility issues.
Comparing clomiphene to other fertility drugs, such as gonadotropins or injectable medications, reveals a trade-off between effectiveness and potential risks or side effects. While more potent drugs may have higher success rates, they also carry a higher risk of ovarian hyperstimulation syndrome (OHSS) and multiple pregnancies, which can lead to complications.
Ultimately, a personalized approach that considers individual circumstances, medical history, and preferences is crucial in determining the most appropriate fertility treatment option. Consulting with a reproductive endocrinologist and carefully weighing the potential benefits and risks is essential for maximizing the chances of a successful pregnancy outcome.
